Monkeypox Outbreak: An Emerging Global Health Concern
Introduction
Monkeypox, a viral zoonotic disease, has recently become a significant public health concern due to its unexpected outbreaks in regions outside its traditional endemic areas. The disease, which was first identified in humans in 1970 in the Democratic Republic of Congo, is caused by the monkeypox virus, a member of the Orthopoxvirus genus, closely related to the viruses causing smallpox and cowpox. Although monkeypox has been historically confined to parts of Central and West Africa, recent outbreaks have highlighted the potential for global spread, necessitating an urgent and coordinated response.
Origins and Transmission
The monkeypox virus is primarily transmitted to humans from animals, particularly rodents and primates, through direct contact with blood, bodily fluids, or skin lesions of infected animals. Human-to-human transmission occurs through respiratory droplets, close physical contact, or contact with contaminated materials such as bedding or clothing. Unlike smallpox, which was eradicated in 1980, monkeypox is less contagious, but it remains a concern due to its potential to cause outbreaks, especially in populations with little immunity to orthopoxviruses.
Symptoms and Clinical Presentation
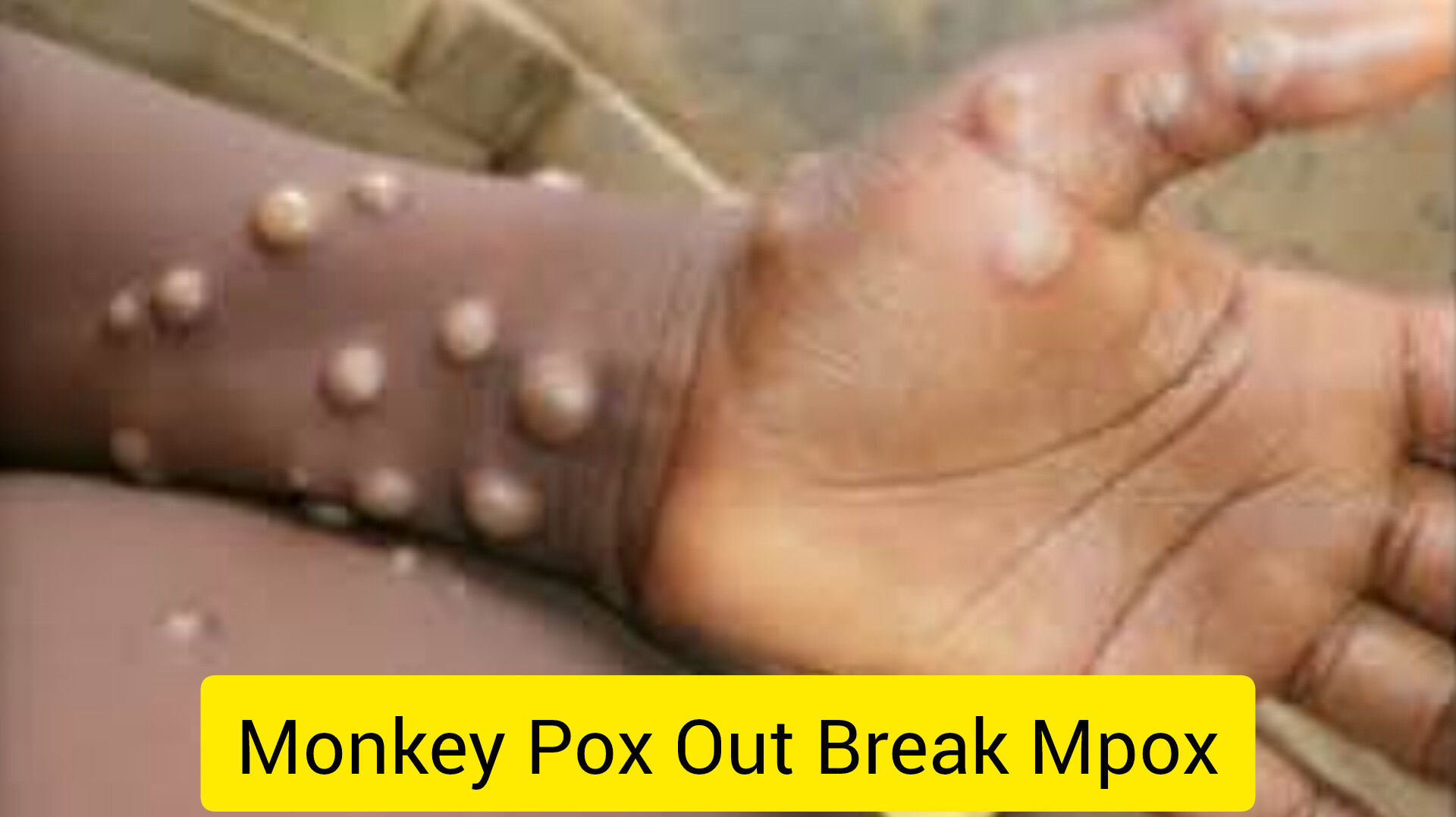
The incubation period of monkeypox typically ranges from 6 to 13 days but can extend to 21 days. The disease often begins with nonspecific symptoms such as fever, headache, muscle aches, and fatigue, followed by the development of a characteristic rash. The rash usually starts on the face before spreading to other parts of the body, including the palms and soles. Lesions progress through several stages—from macules to papules, vesicles, pustules, and eventually scabs—before falling off.
Monkeypox is generally a self-limiting disease, with symptoms lasting 2 to 4 weeks. However, severe cases can occur, particularly in children, pregnant women, and individuals with compromised immune systems. Complications may include secondary bacterial infections, respiratory distress, and, in some cases, encephalitis. The case fatality rate for monkeypox varies, with the West African strain being less severe (1% mortality) compared to the Central African strain, which can have a fatality rate of up to 10%.
Global Spread and Recent Outbreaks
In 2022, the global health community was alarmed by a significant outbreak of monkeypox in multiple countries outside Africa, including Europe, North America, and parts of Asia. This was unusual as previous cases outside Africa were mostly linked to travel or imported animals. The outbreak was characterized by clusters of cases among people with no direct travel history to endemic regions, indicating potential community transmission.
The 2022 outbreak was particularly notable for its occurrence among men who have sex with men (MSM), raising concerns about sexual transmission, although the virus is not primarily classified as a sexually transmitted infection (STI). The World Health Organization (WHO) and other public health agencies quickly responded by issuing guidelines for diagnosis, treatment, and isolation to control the spread.
Diagnosis and Treatment
Diagnosis of monkeypox can be challenging due to its similarity to other rash-causing illnesses such as chickenpox, measles, and bacterial skin infections. Laboratory confirmation is typically achieved through polymerase chain reaction (PCR) testing, which can detect viral DNA from lesion samples. Serological tests can also be used to identify antibodies against the monkeypox virus, but these are less specific and not useful for acute diagnosis.
There is no specific antiviral treatment for monkeypox, although antivirals developed for smallpox, such as tecovirimat, have shown promise in treating monkeypox infections. Supportive care, including hydration, pain management, and treatment of secondary infections, is the mainstay of therapy. Vaccination with the smallpox vaccine has been found to provide cross-protection against monkeypox, and in response to the 2022 outbreak, some countries have begun using the vaccine in high-risk populations.
Prevention and Public Health Measures
Preventing the spread of monkeypox involves a combination of public health measures. In endemic regions, controlling animal reservoirs through safe handling practices and educating the public about the risks of contact with wild animals are crucial. In healthcare settings, strict infection control practices, including the use of personal protective equipment (PPE) and isolation of suspected cases, are essential.
Vaccination plays a critical role in preventing monkeypox. The smallpox vaccine, which was used during the eradication of smallpox, provides around 85% protection against monkeypox. In the wake of recent outbreaks, some countries have reintroduced smallpox vaccination for high-risk groups, including healthcare workers and laboratory personnel. The use of a newer, non-replicating smallpox vaccine, Imvanex (also known as Jynneos in the U.S.), has been authorized for emergency use in controlling monkeypox outbreaks.
Challenges and Future Outlook
The re-emergence of monkeypox as a global health threat underscores the challenges of managing zoonotic diseases in an interconnected world. The recent outbreaks outside Africa highlight the need for improved surveillance, rapid diagnostic capabilities, and a better understanding of the virus’s transmission dynamics. The role of international travel, changes in human behavior, and potential animal reservoirs in non-endemic regions remain areas of active research.
Moreover, the monkeypox outbreaks have reignited discussions about the importance of maintaining preparedness for emerging infectious diseases, especially those with the potential for international spread. Public health authorities must prioritize vaccination strategies, public awareness campaigns, and robust health systems capable of responding swiftly to future outbreaks.
Conclusion
The monkeypox outbreaks of recent years have brought attention to a previously neglected disease, reminding the global community of the ongoing threat posed by zoonotic viruses. While the disease is not as contagious or deadly as smallpox, its potential to cause significant morbidity and its spread to new regions warrant continued vigilance. Strengthening global surveillance, enhancing public health preparedness, and ensuring access to vaccines and treatments are crucial steps in mitigating the impact of future monkeypox outbreaks.